Glaucoma is the most serious eyesight threatening condition. It usually manifests as a painless, gradual loss of vision. The lost vision can never be recovered. However, medical or surgical treatment can prevent or retard further loss of vision.
DR DUDHBHATENETRALAY AND RETINA CENTER CORRECTS GLOUCOMA SYMPTOMS LIKE SEEING BLACK DOTS AND BLURRING OF VISION
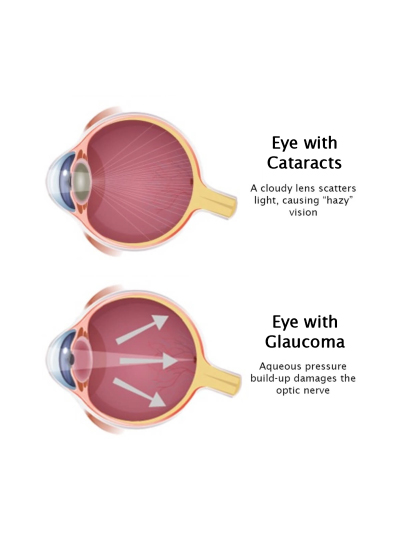
Many times it can be confused with a cataract which also manifests as a painless, gradual loss of vision. The difference is that in the case of cataract, the loss of vision is fully recoverable using a simple surgery called Phaco.
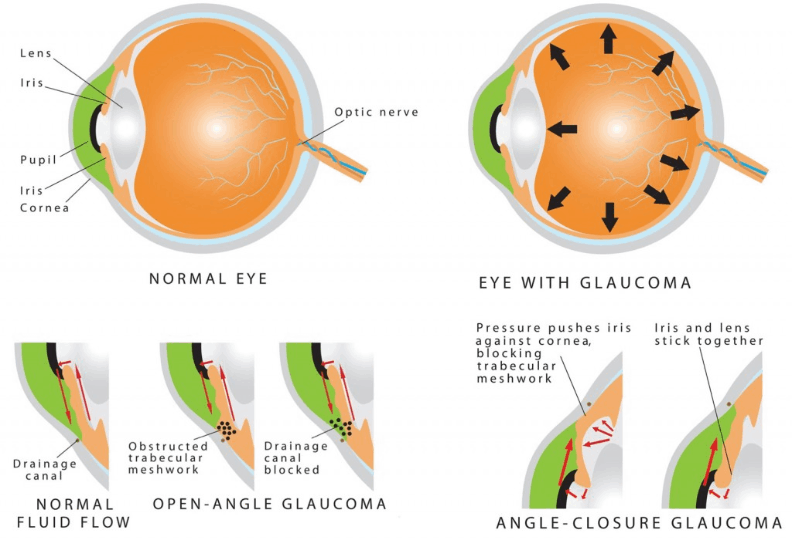
Our eyes contain a clear fluid called aqueous humor, which is continuously produced in the eye to bath and nourish the structures inside it. The fluid normally drains out of the eye through drainage canals in a fine meshwork located around the edge of the iris (the colored part of the eye that surrounds the pupil). In people with glaucoma, the fluid fails to drain due to some defect and thus increases the pressure inside the eyes called raised Intraocular Pressure (IOP) (or Tension).
WHO IS AT A RISK FOR GLAUCOMA?
Anyone can develop glaucoma. Some people are at higher risk than others. They include:
- Diabetics
- People with Migraine
- People with Hypertension
- Everyone over the age of 40 yrs.
- People with family history of glaucoma.
- People with near sightedness (Myopia) for open angle type and far sightedness (hyperopia) for close angle type
GENERAL SYMPTOMS OF GLAUCOMA
Once the lens is removed, it may be replaced by one of the three options :
- Reduced vision in dim illumination and during nights
- Gradual decrease of side vision with the progression of glaucoma
- Frequent change of reading glasses, headaches, pain, and redness of the eyes
- Coloured halo rings seen around light bulbs especially in the mornings and nights
- Pain around the eyes when coming out from darkness (e.g., as soon as the person comes out of a cinema hall)
TYPES OF GLAUCOMA
-
Open Angle Glaucoma
It happens when the eye’s drainage canals become clogged over time. The inner eye pressure (also called intraocular pressure or IOP) rises because the correct amount of fluid can’t drain out of the eye. With open-angle glaucoma, the entrances to the drainage canals are clear and open. The clogging problem occurs further inside the drainage canals, similar to a clogged pipe below the drain in a sink. Most people have no symptoms & no early warning signs. If open-angle glaucoma is not diagnosed & treated, it can cause a gradual loss of vision. This type of glaucoma develops slowly and sometimes without noticeable sight loss for many years. It usually responds well to medication, especially if caught early and treated. This form of glaucoma is more common in Caucasians than others. -
Angle-Closure Glaucoma
This type of glaucoma is also known as acute glaucoma or narrow-angle glaucoma. It is more common in Asians and is very different from open-angle glaucoma in which the eye pressure usually rises very quickly. It happens when the entrance to the drainage canals is very narrow or covered over, like a sink with something covering the drain. Symptoms of angle closure glaucoma may include headaches, eye pain, nausea, rainbows around lights at night, and very blurred vision. -
Low-Tension or Normal-Tension Glaucoma
In this type of glaucoma, the optic nerve is damaged even though intraocular pressure (IOP) is not very high. Lowering eye pressure by at least 30 percent through medicines slows the disease in some people. A comprehensive medical history is essential in identifying other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma. -
Congenital Glaucoma
Children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have visible symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines may have unknown effects in infants and be difficult to administer. The operation is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision. -
Secondary Glaucoma Types
These can develop as complications of other medical conditions. These types of glaucoma are sometimes associated with eye surgery or advanced cataracts, eye injuries, certain eye tumors, or uveitis (eye inflammation). Pigmentary glaucoma occurs when pigment from the iris flakes off and blocks the meshwork, slowing fluid drainage. A severe form, called neo vascular glaucoma, is linked to diabetes. Corticosteroid drugs used to treat eye inflammations, and other diseases can trigger glaucoma in some people. Treatment includes medicines, laser surgery, or conventional surgery. -
Standard Investigation for Glaucoma
Early detection, through regular and complete eye exams, is the key to protecting your vision from damage caused by glaucoma. Following are the ways through which you can get your eyes examined for Glaucoma :
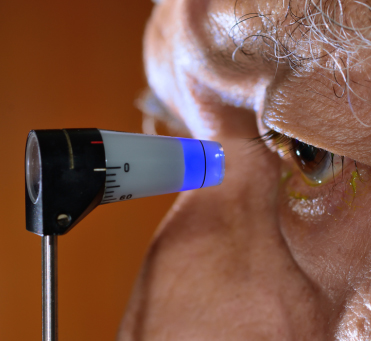
APPLANATION TONOMETRY
The tonometry test measures the inner pressure of the eye. Usually drops are used to numb the eye. Then the doctor or technician will use a special device that measures the eye’s pressure.
OPHTHALMOSCOPY
Ophthalmoscopy is used to investigate the inside of the eye, especially the optic nerve. In a darkened room, the doctor will magnify your eye by using an ophthalmoscope (an instrument with a small light on the end). It helps the doctor look at the shape and color of the optic nerve.

PERIMETRY
Perimetry is a procedure where the patient wears a patch over one eye and looks straight ahead at a bowl-shaped white area. At the same time, the computer presents lights in fixed locations around the bowl. The patient indicates each time he or she sees the light, which is why perimetry can provide a map of the visual fields. The type of vision loss associated with glaucoma is relatively specific, & perimetry can detect the typical visual-field defects of glaucoma disorder. The perimetry test is also called a visual field test.

RETINAL NERVE FIBRE ANALYSIS/OCT
PACHYMETRY
Pachymetry is the method of measuring the thickness of the cornea. Corneal thickness is critical because it can mask an accurate reading of eye pressure, causing doctors to treat you for a condition that may not really exist or to treat you unnecessarily when are normal. Actual IOP may be underestimated in patients with thinner CCT and overestimated in patients with thicker CCT. Pachymetry is a simple, quick, painless test With this measurement; your doctor can better understand your IOP reading, and develop a treatment plan that is right for your condition. The procedure takes only about a minute to measure both eyes.

RETINAL NERVE FIBRE ANALYSIS/OCT
Glaucoma is a chronic and progressive condition. Any vision loss that had occurred, before glaucoma was diagnosed, cannot be reversed. Glaucoma treatments at Dr. Dudhabhate Netralaya and Retina Centre include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma..
Medicines, in the form of eye drops or pills, are the most common early treatment for glaucoma. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye. Glaucoma medicines may be taken several times a day. You need to use the drops or pills as long as they help control your eye pressure. Regular use is essential.
Laser trabeculoplasty helps fluid drain out of the eye. Your doctor may suggest this step at any time. In many cases, you need to keep taking glaucoma drugs after this procedure. It is performed in your doctor’s office or eye clinic.
Conventional surgery makes a new opening for the fluid to leave the eye. Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines, and laser surgery has failed to control pressure.
FAQS ABOUT GLAUCOMA TREATMENT
Not necessarily. Increased eye pressure means you are at risk for glaucoma but does not mean you have the disease. A person has glaucoma only if the optic nerve is damaged. If you have increased eye pressure but no damage to the optic nerve, you do not have glaucoma.
- If you have a family history of glaucoma
- If you experience blurring of vision
- If you see haloes around light
- If you suffer from frequent headaches
- Frequent change of glasses due to decreasing eyesight.
A glaucoma suspect is a person in who, in the doctor’s opinion, there is a high chance of developing glaucoma. It may be due to the elevated eye pressure or the appearance of the optic nerves. Some people may have pressures that are higher than normal, but is not associated with optic nerve damage and vision loss but they do not develop glaucoma and are called ocular hyper-tensives. Other people have optic nerves that might appear to be abnormal, but, in fact, are normal for them.
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another. Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important.
A glaucoma suspect is a person in who, in the doctor’s opinion, there is a high chance of developing glaucoma. It may be due to the elevated eye pressure or the appearance of the optic nerves. Some people may have pressures that are higher than normal, but is not associated with optic nerve damage and vision loss but they do not develop glaucoma and are called ocular hyper-tensives. Other people have optic nerves that might appear to be abnormal, but, in fact, are normal for them.
There is usually no visible scarring but at times the white of the eye
can have any degree of redness
You may go home with an eye pad and
shield, or just a shield. The pad can be removed after the first hour.
The shield should be worn at night for the first week.
Your vision
will normally be much better by Day 2. Sometimes there can be some
blurring or misting in the eye, but this should improve over the course
of the day. If you feel your vision is becoming more blurred, contact
your hospital immediately.
- If you have a family history of glaucoma
- If you experience blurring of vision
- If you see haloes around light
- If you suffer from frequent headaches
- Frequent change of glasses due to decreasing eyesight.
If you are over age 60, diabetic or have a family member with glaucoma, you are at higher risk for glaucoma than others. Risk factors for glaucoma, rest will reach you one by one



